Table Of Content
The House Brackmann scale has also been criticized for insufficient correlation with best or worst function in the studied domains. The scale was created in 1985, by Dr John W. House and Dr Derald E. Brackmann, otolaryngologists from California. Please note that once you have closed the PDF you need to click on the Calculate button before you try opening it again, otherwise the input and/or results may not appear in the pdf.
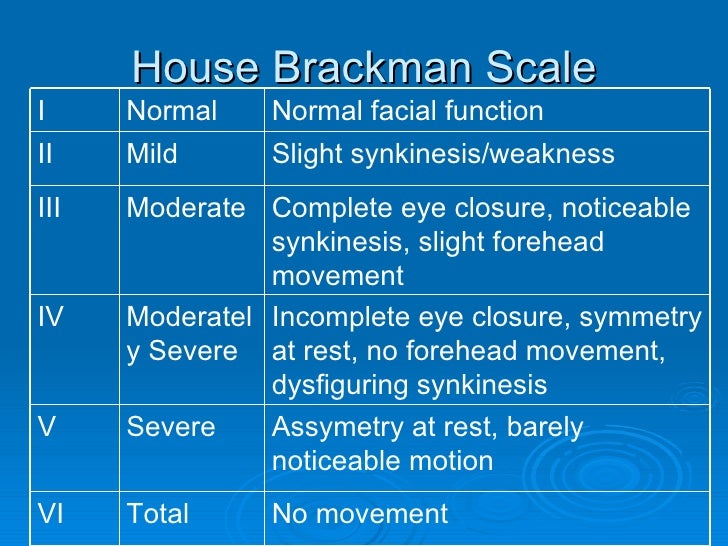
HOUSE-BRACKMANN FACIAL PARALYSIS SCALE
The Sunnybrook scale is another facial paralysis grading system used in lieu of or in conjunction with the House-Brackmann scale. With the Sunnybrook scale, a single score is generated that accounts for primary and secondary facial defects. The House-Brackmann grading system can be used to evaluate these symptoms, but additional testing is usually required to assess their severity.
The use of basic fibroblast growth factor to treat intractable Bell's palsy administered via transcanal endoscopic ear ... - ScienceDirect.com
The use of basic fibroblast growth factor to treat intractable Bell's palsy administered via transcanal endoscopic ear ....
Posted: Sat, 12 Aug 2023 14:02:42 GMT [source]
House-Brackmann facial paralysis scale
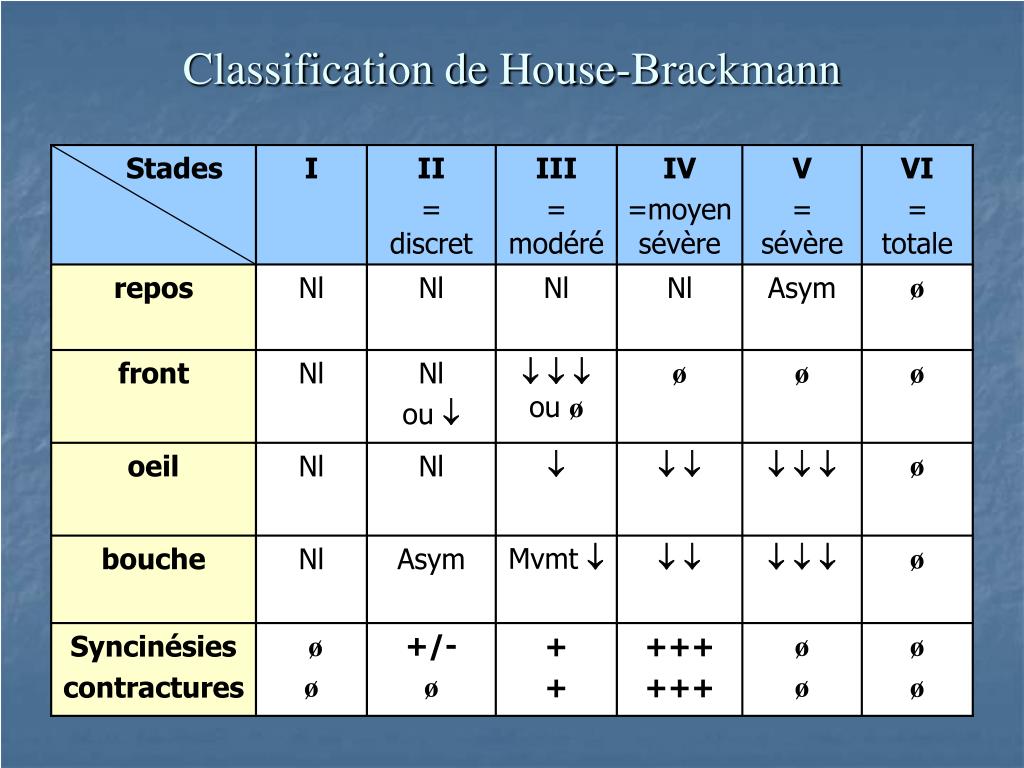
At the Sorensen Clinic we routinely use the House-Brackmann scale to evaluate new and existing patients. In addition we include a description of segmental weakness (zone-specific information), changes in the facial soft tissues and synkinesis. House-Brackmann (HB) is one of several analysis tools developed to quantify facial function and provide reproducible information. It is a widely accepted system, simple, sensitive, accurate and reliable - grading facial function in six steps from normal (HB I) to total paralysis (HB VI). Many of these symptoms will change over time, for example following a spontaneous recovery of nerve function or as a result of different therapeutic modalities (i.e after surgical treatment). There are 6 grades in this scale, that are assigned Roman numbers from I to VI, I indicating normal function while VI is suggestive of complete paralysis.
Motion function: Mouth
The highest correlation of the overall grading is with the regional scoring of the eye at 61% while the lowest is with the forehead region at 18%. The House-Brackmann score carries the name of the Dr John W. House and Dr Derald E. Brackmann, otolaryngologists in Los Angeles, California, who first described the system in 19851). The contents of this web site are for information purposes only, and are not intended to be a substitute for professional medical advice, diagnosis, or treatment.
Temporalis Muscle Transposition in Irreversible Facial Nerve Palsy: A Vestibular Approach - Cureus
Temporalis Muscle Transposition in Irreversible Facial Nerve Palsy: A Vestibular Approach.
Posted: Sat, 30 Dec 2023 08:00:00 GMT [source]
All House-Brackmann classification scores are made based on eyebrow and mouth movement on the non-paralyzed side of a patient’s face. Symptoms of facial nerve injury may vary due to age, facial anatomy and the extent of nerve-damage. Frequent patient concerns relate to brow position, movement abnormalities, eyelid closure issues, inability to smile, mid-facial asymmetries, poor oral function and lower lip asymmetry. The House-Brackmann Facial Nerve Grading System is widely used to characterize the degree of facial paralysis. In this scale, grade I is assigned to normal function, and grade VI represents complete paralysis. A light degree of facial nerve weakness may only be visible as subtle asymmetries following repeated and exhausting muscle function, whereas severe dysfunction can be easily recognised even at rest.
Iowa Head and Neck Protocols
The House–Brackmann score is a score to grade the degree of nerve damage in a facial nerve palsy. The measurement is determined by measuring the upwards (superior) movement of the mid-portion of the top of the eyebrow, and the outwards (lateral) movement of the angle of the mouth. Each reference point scores 1 point for each 0.25 cm movement, up to a maximum of 1 cm. The Burres-Finch system is a House-Brackmann grading scale alternative that was designed to minimize subjectivity. It involves the use of a continuous graded scale of linear measurements of different reference points across a facial paralysis patient’s face. These measurements were used to produce electromyographic recordings and provided objective insights into the severity of a patient’s facial paralysis symptoms.
Along with the Burres-Finch system, the Nottingham system has been used as a House-Brackmann scale alternative. Like the Burres-Finch system, the Nottingham system focused on providing an objective look at a patient’s facial paralysis symptoms. The Nottingham system also includes criteria designed to provide insights into secondary facial defects. Whatever the cause, the consequences for the patient can be devastating depending on the level of facial dysfunction. Several modalities exist to clinically rate the degree of facial function; including the widely used House-Brackman classification.
Facial Paralysis House Brackmann Scale
Welcome to the Facial Paralysis Institute, your premier destination for comprehensive facial paralysis treatment. Our expert team provides exceptional care and specialized solutions for individuals suffering from facial paralysis. We offer a wide range of services to help restore your facial nerve function and improve your quality of life, from facial paralysis reanimation surgery to acoustic neuroma treatment, etc. Located in Los Angeles, California, we proudly serve patients from not only the United States but also from around the world. Whether you're seeking treatment locally or traveling from afar, our compassionate team is here to guide you on your journey to facial restoration.
House-Brackmann Classification of Facial Function
The House-Brackmann scale for Bell’s Palsy or other forms of facial paralysis can be used to measure the severity of a patient’s symptoms, but it offers no guarantees. Facial paralysis symptoms vary, and a patient requires an in-depth evaluation to determine why these symptoms are occurring and what can be done to correct them and prevent them from recurring. It is therefore crucial for a facial paralysis patient to meet with an expert facial paralysis and reconstructive surgeon, like Dr. Babak Azizzadeh of The Facial Paralysis Institute to discuss their symptoms. Furthermore, the House-Brackmann scale does not account for the fact that facial paralysis symptoms may be more severe in certain parts of the face than others, too.
Facial paralysis can result from trauma, infection, congenital, metabolic, neoplastic, toxic, iatrogenic, or idiopathic etiologies.
We specialise in plastic surgery, cosmetic surgery, reconstructive surgery of the face, microsurgery, eyelid and oculoplastic surgery, facial nerve surgery, breast surgery and breast augmentation. The function of facial muscles is essential in mastication, speech and emotion expression, therefore facial nerve injury, either complete or partial is of important concern because it can result in facial paralysis. During a first consultation with Dr. Azizzadeh, a facial paralysis patient will receive a full evaluation. Then, Dr. Azizzadeh offers a personalized treatment plan to help his patient address their facial paralysis symptoms.
The University of Iowa does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on this web site. Although the standards discussed herein reflect the University of Iowa's head and neck protocols, reliance on any information provided herein is solely at your own risk. The Department of Otolaryngology and the University of Iowa wish to acknowledge the support of those who share our goal in improving the care of patients we serve. The University of Iowa appreciates that supporting benefactors recognize the University of Iowa's need for autonomy in the development of the content of the Iowa Head and Neck Protocols.

No comments:
Post a Comment